Resumen
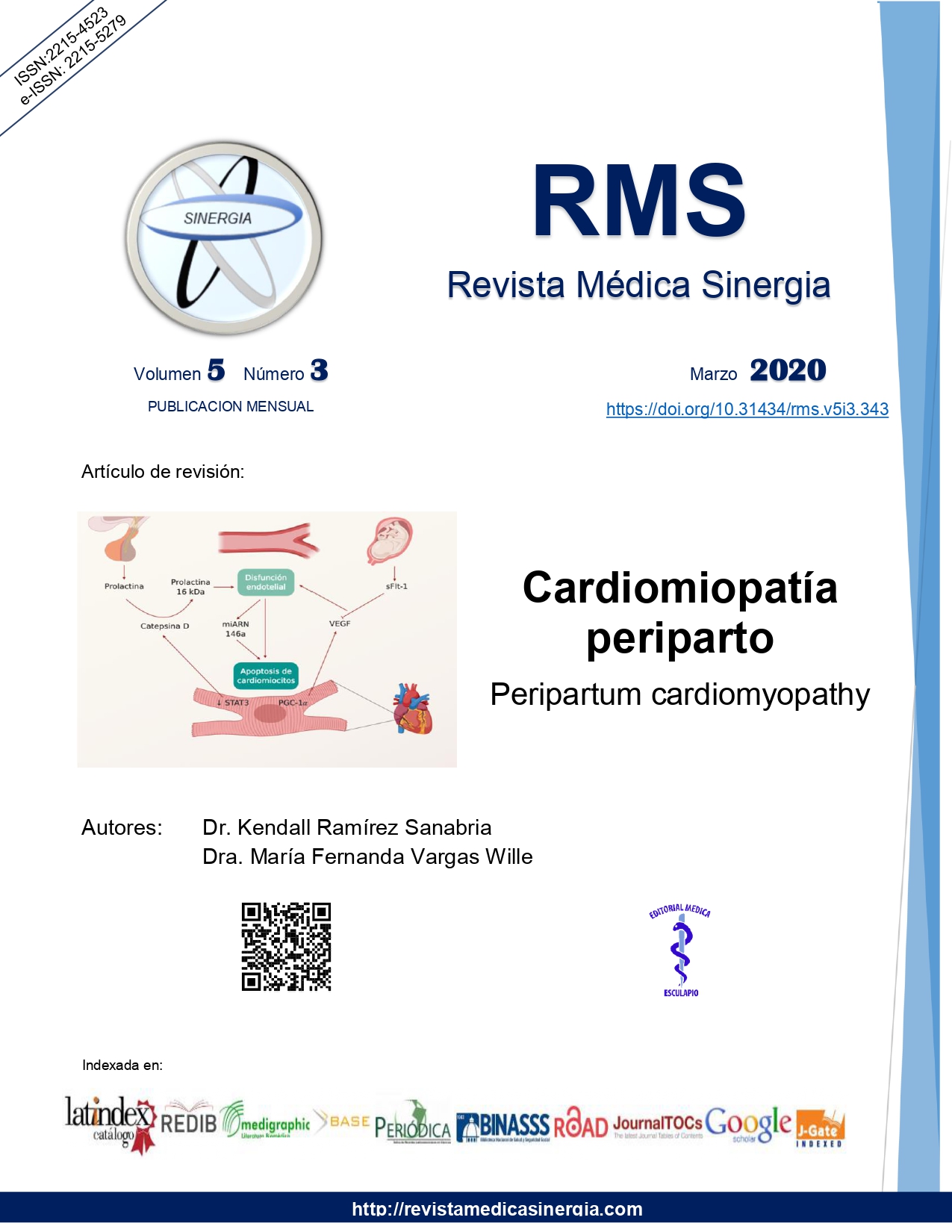
La cardiomiopatía periparto (CPP) es una cardiomiopatía con disfunción sistólica que se presenta usualmente al final del embarazo y en las primeras semanas del periodo postparto. Los factores de riesgo incluyen etnia afrodescendiente, hipertensión gestacional, preeclampsia, edad materna mayor a 30 años y gestación múltiple. Se han dilucidado varios mecanismos fisiopatológicos implicados en el desarrollo de la CPP tales como un aumento de la prolactina, una disminución en factores transcripcionales antioxidantes como el STAT3 y un aumento de proteínas producidas en la placenta como el sFlt-1, lo que en conjunto produce disfunción endotelial y apoptosis de los cardiomiocitos. La CPP es un diagnóstico de exclusión, por lo que en una mujer con clínica de insuficiencia cardiaca en el periodo periparto se debe descartar otras causas como la cardiomiopatía dilatada o valvular preexistente, infarto agudo del miocardio y tromboembolismo pulmonar. Actualmente el tratamiento se basa en el manejo básico de la insuficiencia cardiaca, además de soporte hemodinámico en caso de ser necesario.
Citas
Cunningham FC, Byrne JJ, Nelson DB. Peripartum cardiomyopathy. Obstet Gynecol. 2019; 133:167-79. https://doi.org/10.1097/AOG.0000000000003011.
Arany Z, Elkayam U. Peripartum cardiomyopathy. Circulation. 2016; 133:1397-1409. https://doi.org/10.1161/CIRCULATIONAHA.115.020491.
Honigberg MC, Givertz M. Peripartum cardiomyopathy. BJM. 2019; 364:k5287. https://doi.org/10.1136/bmj.k5287.
Sliwa K, Hilfiker-Kleiner D, Petrie MC, et al. Current state of knowledge on aetiology, diagnosis, management, and therapy of peripartum cardiomyopathy: a position statement from the Heart Failure Association of the European Society of Cardiology Working Group on peripartum cardiomyopathy. Eur J of Heart Failure. 2010; 12:767-778. https://doi.org/10.1093/eurjhf/hfq120.
Koenig T, Hilfiker-Kleiner D, Bauersachs J. Peripartum cardiomyopathy. Herz. 2018; 43: 431-37. https://doi.org/10.1007/s00059-018-4709-z.
Karaye KM, et al. Serum Selenium and ceruloplasmin in nigerians with peripartum cardiomyopathy. Int J Mol Sci. 2015; 16(4): 7644-54. https://doi.org/10.3390/ijms16047644.
Main EK, McCain CL, Morton CH, Holtby S, Lawton ES. Pregnancy-related mortality in California: causes, characteristics, and improvement opportunities. Obstet Gynecol. 2015;125:938-47. https://doi.org/10.1097/AOG.0000000000000746.
Sliwa K, Mebazaa A, Hilfiker-Kleiner D, et al. Clinical characteristics of patients from the worldwide registry on peripartum cardiomyopathy (PPCM). Eur J of Heart Failure. 2017; 19:1131-41. https://doi.org/10.1002/ejhf.780.
Afana M, Brinkikji W, Kao D, et al. Characteristics and in-hospital outcomes of peripartum cardiomyopathy diagnosed during delivery in the United States from The Nationwide Inpatient Sample (NIS) Database. J Card Fail. 2016; 22:512-9. https://doi.org/10.1016/j.cardfail.2016.02.008.
Schelbert EB, Elkayam U, Cooper LT, et al. Myocardial damage detected by late gadolinium enhancement cardiac magnetic resonance is uncommon in peripartum cardiomyopathy. J Am Heart Assoc. 2017; 6:e005472. https://doi.org/10.1161/JAHA.117.005472.
Harhous Z, Booz G, Ovize M, Bidaux G, Kurdi M. An update on the multifaceted roles of STAT3 in the heart. Front Cardiovasc Med. 2019; 6:1-18. https://doi.org/10.3389/fcvm.2019.00150.
Naftali-Shani N, et al. Modeling peripartum cardiomyopathy with human induced pluripotent stem cells reveals distinctive abnormal function of cardiomyocytes. Circulation. 2018; 138:2721-23. https://doi.org/10.1161/CIRCULATIONAHA.118.035950.
Ware JS, Li J, Mazaika E, et al. Shared genetic predisposition in peripartum and dilated cardiomyopathies. N Engl J Med. 2016; 374:233-41. https://doi.org/10.1056/NEJMoa1505517.
Honigberg MC, Givertz MM. Arrhythmias in peripartum cardiomyopathy. Card Electrophysiol Clin. 2015; 7:309-17. https://doi.org/10.1016/j.ccep.2015.03.010.
Bauersachs J, Arrigo M, Hilfiker-Kleiner D, et al. Current management of patients with severe acute peripartum cardiomyopathy: a practical guidance from the Heart Failure Association of the European Society of Cardiology Study Group on peripartum cardiomyopathy. Eur J Heart Fail. 2016; 18:1096-1105. https://doi.org/10.1002/ejhf.586.
Elkayam U, Goland S, Pieper PG, Silverside CK. High-risk cardiac disease in pregnancy: part I. J Am Coll Cardiol. 2016; 68:396-410. https://doi.org/10.1016/j.jacc.2016.05.048.
Ntusi NB, Badri M, Gumedze F, Sliwa K, Mayosi BM. Pregnancy-associated heart failure: a comparison of clinical presentation and outcome between hypertensive heart failure of pregnancy and idiopathic peripartum cardiomyopathy. PLoS One. 2015; 10:e0133466. https://doi.org/10.1371/journal.pone.0133466.
Hilfiker-Kleiner D, Haghikia A, Nonhoff J, Bauersachs J. Peripartum cardiomyopathy: current management and future perspectives. Eur Heart J. 2015; 36(18): 1090-97. https://doi.org/10.1093/eurheartj/ehv009.
Hilfiker-Kleiner D, Haghikia A, Berliner D, et al. Bromocriptine for the treatment of peripartum cardiomyopathy: a multicentre randomized study. Eur Heart J. 2017; 38:2671-9. https://doi.org/10.1093/eurheartj/ehx355.
Arrigo M, Blet A, Mebazaa A. Bromocriptine for the treatment of peripartum cardiomyopathy: welcome on BOARD. European Heart Journal, 38(35), 2680-2682. https://doi.org/10.1093/eurheartj/ehx428.
Nonhoff J, Ricke-Hoch M, Mueller M, et al. Serelaxin treatment promotes adaptive hypertrophy but does not prevent heart failure in experimental peripartum cardiomyopathy. Cardiovasc Resc. 2017; 113:598-608. https://doi.org/10.1093/cvr/cvw245.